VOLUME 13 NUMBER 2 (July to December 2020)
Philipp. Sci. Lett. 2020 13 (2) 95-100
available online: July 31, 2020
*Corresponding author
Email Address: jaibana@up.edu.ph
Date received: July 2, 2020
Date revised: July 28, 2020
Date accepted: July 28, 2020
ARTICLE
Is the value of anti-SARS-CoV-2 IgA antibody detection underappreciated in our current COVID-19 pandemic response?
Ivan Christian VJ. Imperial, Giann Kerwin Y. Dellosa, and Joyce A. Ibana*
1Immunopharmacology Research Laboratory,
Institute of Biology, College of Science,
University of the Philippines, Diliman,
Quezon City, 1101 Philippines
Institute of Biology, College of Science,
University of the Philippines, Diliman,
Quezon City, 1101 Philippines
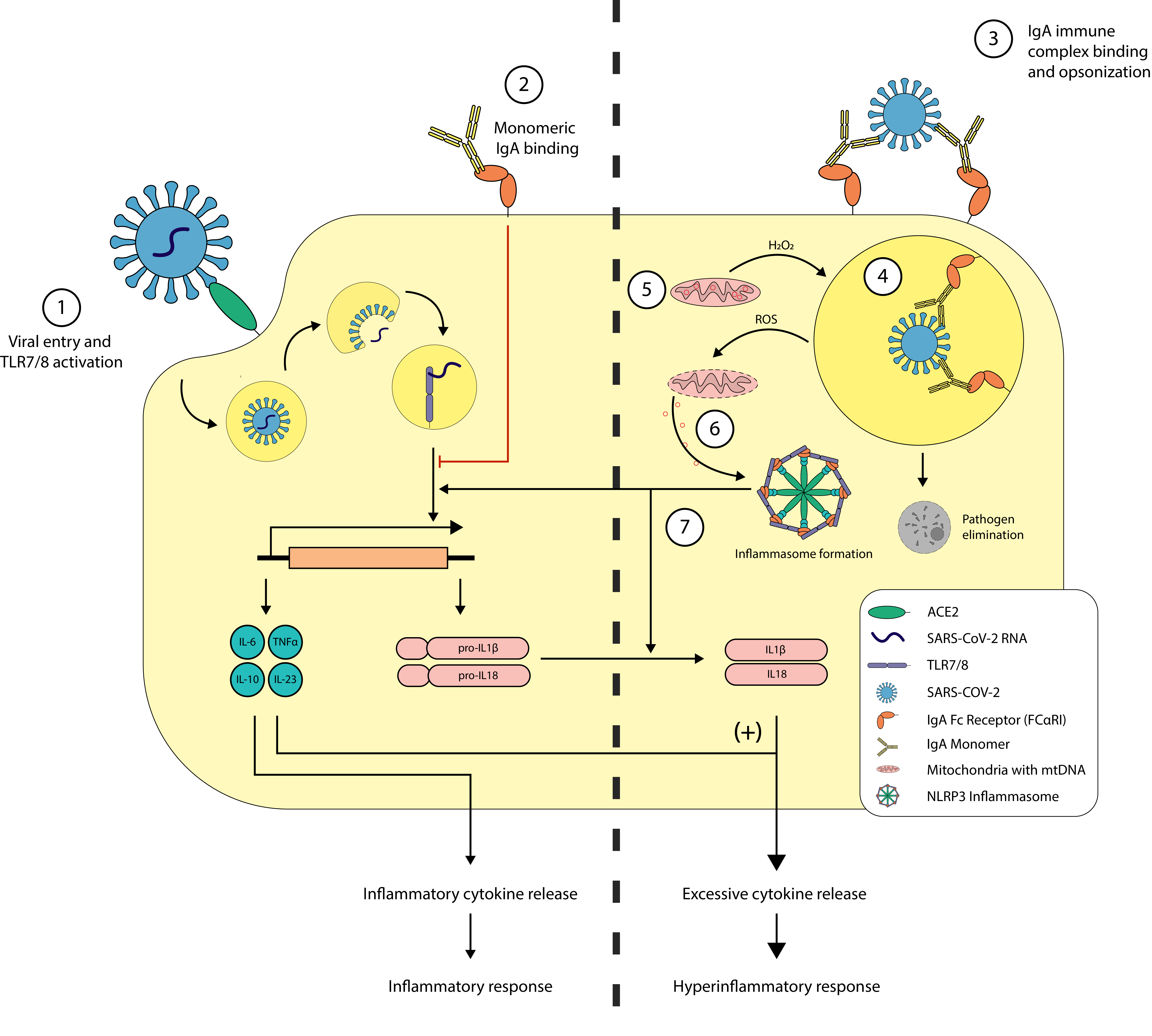
Despite the nature of COVID-19 as a disease of mucosal tissue sites, current serological tests are primarily focused on IgM and IgG antibody detection. The significance of testing for IgA antibody response to SARS-CoV-2 infection and their potential role in COVID-19 disease progression is not yet well explored. Intriguingly, several studies revealed that heightened IgA antibody response to SARS-CoV-2 correlated with COVID-19 disease severity. We hypothesize that the assessment of serum IgA levels can aid in the prognostication of severe COVID-19 progressors. Our hypothesis posits that an IgA antibody response to SARS-COV-2 that is skewed towards Fc binding to CD89 (FcαRI) to form immune complexes (IgA-IC) rather than inhibiting viral entry to host epithelial cells, results in IgA-IC-mediated hyperinflammatory response. The propensity for an elevated non-neutralizing IgA antibody response in sera of COVID-19 patients may lead to the unregulated crosstalk between PRR-induced priming of inflammation and IgA-IC-induced NLRP3 inflammasome formation. Therefore, we believe that looking into the dynamics of the SARS-CoV-2-specific IgA response and their threshold values associated with the clinical severity of COVID-19 warrants further investigations. If our hypothesis is correct, serum IgA may supplement, if not precede, traditional serum diagnostic markers of end-organ damage that are currently used for COVID-19. Investigating the feasibility of using IgA as a biomarker for severe COVID-19 progressors in future studies may reveal its underappreciated value in improving current clinical management and treatment of SARS-CoV-2 positive patients.
© 2024 SciEnggJ
Philippine-American Academy of Science and Engineering