VOLUME 17 (Supplement)
SciEnggJ 17 (Supplement) 362-367
available online: August 31, 2024
DOI: https://doi.org/10.54645/202417SupZJE-41
*Corresponding author
Email Address: mszamora3@up.edu.ph
Date received: February 20, 2024
Date revised: March 14, 2024
Date accepted: March 23, 2024
ARTICLE
The efficacy of methylxanthines as adjunct to standard of care in improving outcomes among chronic obstructive pulmonary disease patients at high risk for and in acute exacerbation: A systematic review and meta-analysis of randomized and non-randomized studies
Philippines – Manila
2Department of Medicine, UP College of College, Manila Philippines
3Department of Medicine, ManilaMed, Manila Philippines
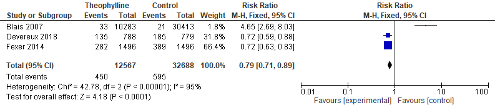
Methylxanthines has established recommendations among stable COPD patients as third line bronchodilator to beta-agonist and anti-cholinergics. However, data on its recommendation as an adjunct in exacerbation and its utility in preventing exacerbation among high risk patients remain scarce and conflicting. A systematic review and meta-analysis was performed on all randomized and non-randomized control trials determining association between the addition of methylxanthines to standard of care in improving outcomes in 1) high risk patients 2) patients in exacerbation. Two reviewers independently studied and reviewed the articles for quality. The following data extracted from the studies included: incidence of COPD exacerbation in one year, exacerbation requiring hospitalization, breathlessness score/quality of life score and inflammatory indices. A total of 7 studies were included in the final study. Pooled analysis of data showed that methylxanthines were associated with lower risk of exacerbations requiring hospitalization after 1 year of treatment (RR 0.79, [95% CI 0.71, 0.89]) and improved anti-inflammatory response by increasing histone deacetylase (HDAC) activity. However, it did not show statistical difference on the incidence of COPD exacerbation after 1 year (RR 0.94, [95% CI 0.86, 1.02]) nor improvement in breathlessness score/quality of life score. Looking at adverse events, methylxanthines were not associated with an increased risk (RR 2.69, CI 0.29, 26.9 I2 65%) of palpitations and regurgitation. The systematic review and meta-analysis showed that methylxanthines have utility in increasing HDAC and decreasing hospital related admissions due to exacerbation without additional adverse events. However, it does not decrease risk of exacerbation, self-reported symptom score and quality of life.
© 2026 SciEnggJ
Philippine-American Academy of Science and Engineering