VOLUME 18 (Supplement)
SciEnggJ 18 (Supplement) 469-482
available online: 11 December 2025
DOI: https://doi.org/10.54645/202518SupIFI-95
*Corresponding author
Email Address: arsy3@outlook.up.edu.ph
Date received: 02 September 2025
Dates revised: 16 November 2025
Date accepted: 24 November 2025
ARTICLE
Flexible decay metrics for early prediction of gestational trophoblastic neoplasia: A comparative modeling approach
University of the Philippines Manila, Manila, Philippines 1000
2Department of Pharmacology and Toxicology, College of Medicine,
University of the Philippines Manila, Manila, Philippines 1000
3Department of Health Policy and Administration, College of Public
Health, University of the Philippines Manila, Manila, Philippines
1000
4Department of Physiology, College of Medicine, University of the
Philippines Manila, Manila, Philippines 1000
5School of Statistics, University of the Philippines Diliman, Quezon
City, Philippines 1101
6Section of Trophoblastic Diseases, Department of Obstetrics and
Gynecology, University of the Philippines Philippine General
Hospital, Taft Avenue, Manila, Philippines 1000
Background: Molar pregnancy is a rare condition carrying a 15-22% risk of progression to gestational trophoblastic neoplasia (GTN). Although serial β-hCG monitoring is standard, its ability to predict early malignant change early remains uncertain.
This study examined whether flexible β-hCG decay metrics could improve early GTN prediction compared with conventional thresholds, and whether machine-learning classifiers provide meaningful gains beyond interpretable statistical models.
Methods: This retrospective cohort analyzed 413 post-molar patients with longitudinal β-hCG data. Seven decay metrics were derived from early follow-up measurements and evaluated using logistic and gradient boosting machine (GBM) models.
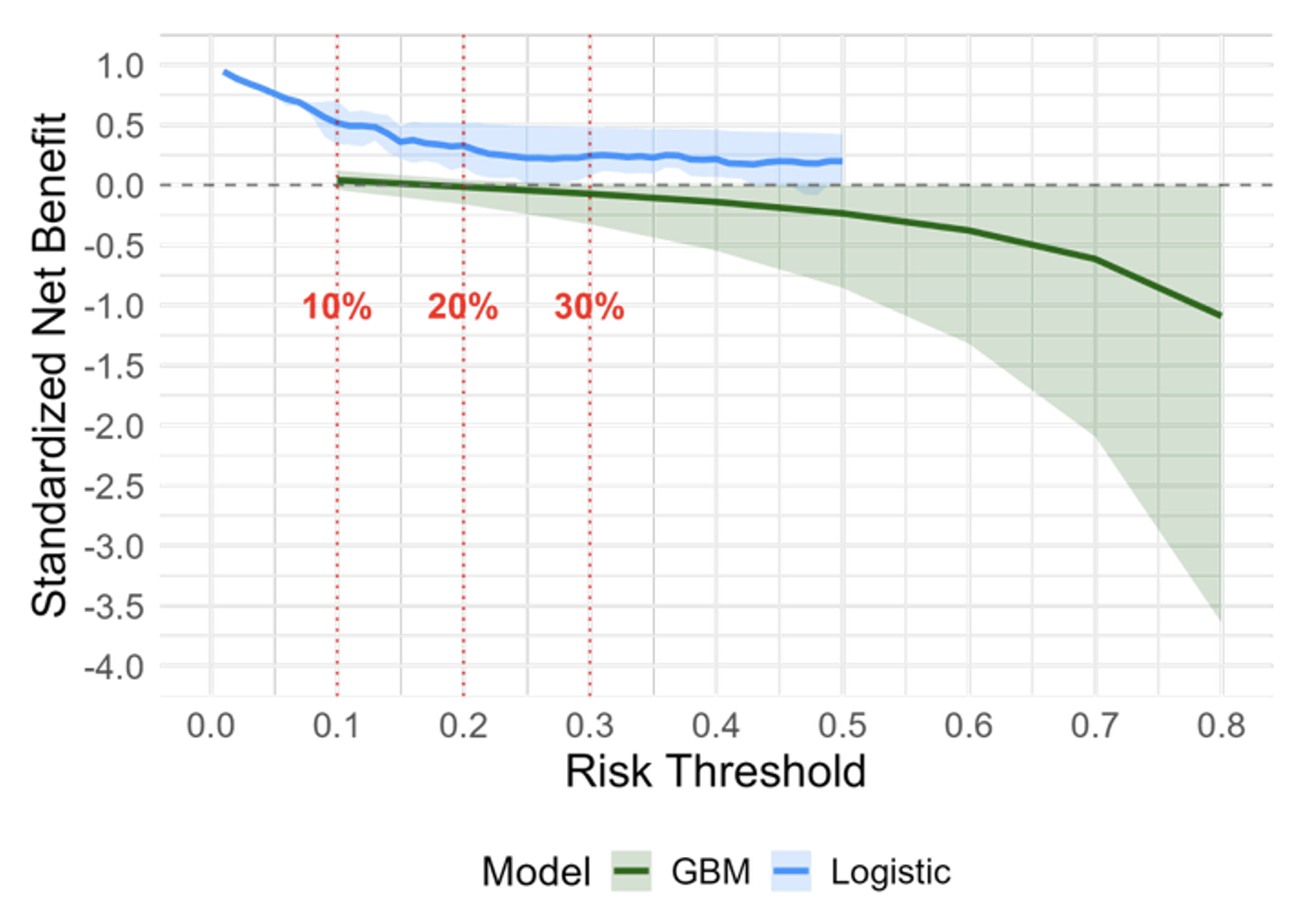
Model performance was assessed through cross-validated discrimination (area under the curve (AUC)), calibration, and decision-curve analysis (DCA).
Results: The GBM model achieved higher apparent discrimination (AUC: 0.96) but negligible net clinical benefit (NCB) across thresholds, indicating probable overfitting and limited bedside utility. A parsimonious logistic model (AUC: 0.77; calibration slope: 0.85) showed stable calibration and consistent net benefit for identifying low-risk patients. Among the decay metrics, time-to-75% β-hCG decline (~25 days) emerged as the most robust and interpretable predictor (sensitivity 92%, negative predictive value 88%), offering a simple signal of malignant persistence.
Conclusion: Early β-hCG decay dynamics, particularly time-to-75% decline, can guide risk-adaptive follow-up after molar evacuation. Complex machine-learning models contributed little beyond traditional approaches in this moderate-sized cohort. These findings support prospective validation and exploration of cost-effective surveillance models tailored to resource-limited settings.
© 2026 SciEnggJ
Philippine-American Academy of Science and Engineering